Researchers from Washington University School of Medicine in St. Louis and Northwestern University have taken a monumental step in battling one of the deadliest brain cancers without needing invasive surgery. Their recent findings, showcased in the Proceedings of the National Academy of Sciences, reveal a novel nanotherapy that can be delivered through nasal drops.
This innovative treatment employs specially designed spherical nucleic acids to alter the immune landscape within Glioblastoma tumors, successfully prompting long-term immunity in mice.
Addressing the “Cold Tumor” Issue
Glioblastoma stands out as the most prevalent and lethal type of brain cancer, claiming around three lives per 100,000 individuals annually. It proliferates swiftly, resists conventional treatments, and frequently recurs after intervention. Scientists have labeled this tumor as a “cold tumor” because it skillfully evades detection by the immune system.
To expose this hidden threat, the research team employed a cellular alarm mechanism called cGAS–STING, which typically identifies foreign DNA and instigates an inflammatory response. Although available drugs can technically trigger this alarm, existing treatments often break down too swiftly and necessitate risky injections directly into the brain.
Stéphane Stegh, who led the research at Washington University’s Siteman Cancer Center, expressed the team’s objective: “We aimed to revolutionize cancer treatment by crafting a non-invasive method to activate immune responses against glioblastoma.”
Teaming up with Northwestern’s chemist Chad Mirkin, known for developing spherical nucleic acids—tiny gold particles encased in DNA or RNA strands—proved essential. Together, they refined a version called ISD45-SNAs, which activates cGAS, effectively launching the immune alarm system.
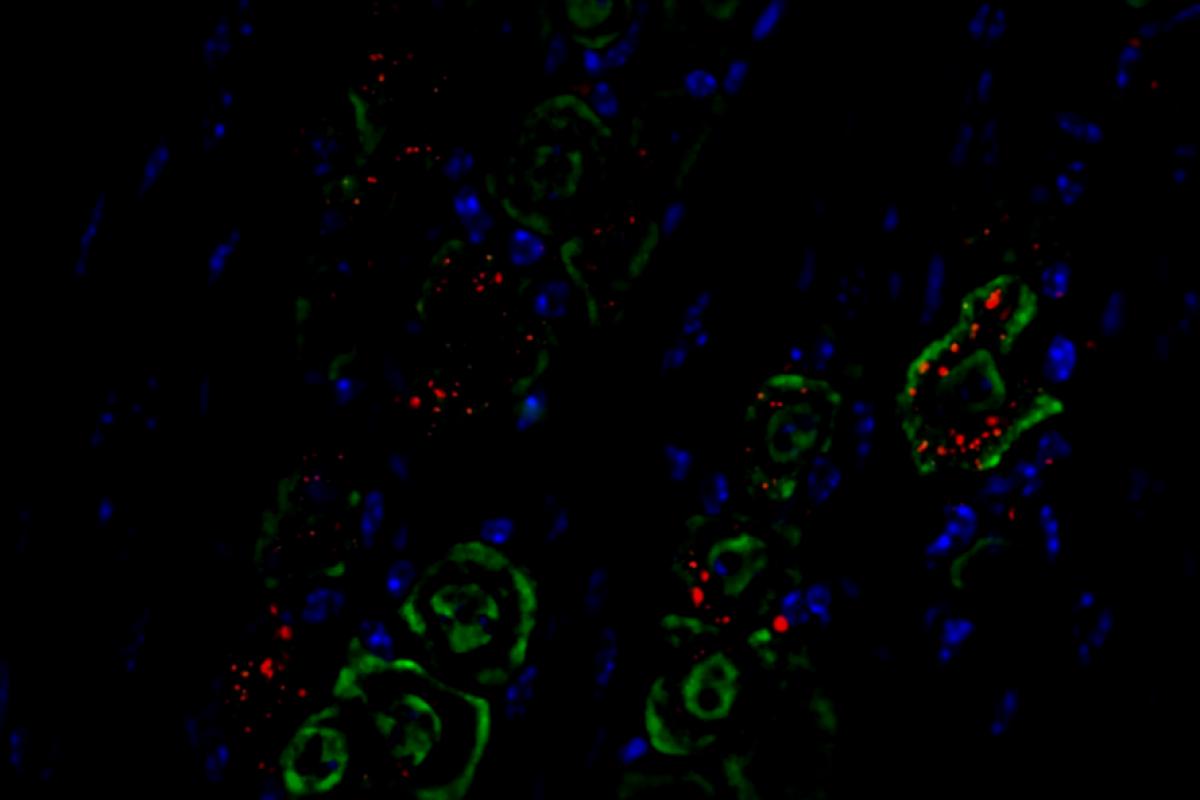
When these nano-particles were administered through the noses of tumor-afflicted mice, they traveled along the trigeminal nerve, the pathway linking the nasal passage to the brain, and concentrated within the tumors. This action prompted macrophages, which usually aid glioblastoma, to switch to a tumor-fighting mode instead.
Importantly, the therapy targeted only the brain, preventing inflammation in other organs.
One Dose for Extended Protection
The outcomes were remarkable; mice receiving the nasal therapy demonstrated a drastically extended lifespan compared to the control group. The results became even more promising when the therapy was combined with checkpoint inhibitors—medications that activate immune cells. Together, they eradicated tumors after just one or two doses.
Stegh conveyed, “Our research indicates that these novel SNAs not only reduce tumor size but also effectively ‘warm up’ an otherwise cold and immunosuppressed tumor environment. This enhancement significantly boosts the efficacy of checkpoint inhibitors.”
Even months later, the treated mice resisted new tumor growth, an indicator that the therapy had conditioned their immune system for long-term combat. This milestone marks a significant achievement in treatment efficacy.
“For the first time, our work demonstrates that we can boost immune cell activation in glioblastoma tumors via nasal delivery of nanoscale therapeutics,” claimed Akanksha Mahajan, the lead author of the study.
Visuals from the research illustrated the pathway: the nanodrops navigated neural routes directly to the tumor, energizing immune cells on their way. Within the cancerous environment, macrophages shifted to a pro-inflammatory state, T cells proliferated, and suppressive immune cells diminished in number. Survival rates in female mice surged nearly threefold.
However, Stegh warned that simply activating the STING pathway is not a catch-all solution for humans at this stage. Glioblastoma employs various techniques to undermine the immune responses that STING aims to activate. The team is now focused on creating nanostructures that can simultaneously engage multiple immune pathways.
A Glimmer of Hope
While the findings are promising, the nasal spray isn’t hitting the shelves of pharmacies anytime soon. The precise delivery of medicine into the human brain via the nasal cavity requires specialized devices and dosing systems that are still in development.
Stegh remarked, “The target product will likely resemble a regular nasal spray, but the formulation and device must be finely tuned for stability, precise dosing, and effective nasal delivery.”
The potential applications of this approach stretch beyond just brain cancer treatment. It may educate the immune system to recognize other types of “cold” tumors, such as those in pancreatic and ovarian cancers.
Stegh concluded, “This approach represents a beacon of hope for creating safer and more effective therapies for glioblastoma and potentially for other immune-resistant cancers.”
This article was originally published on ZME Science. Stay ahead in science by subscribing to our newsletter and keeping updated with the latest breakthroughs.