In a surprising move, an important vaccine advisory group at the Centers for Disease Control and Prevention (CDC) decided to vote against the long-standing recommendation that all newborns receive their first dose of hepatitis B vaccine.
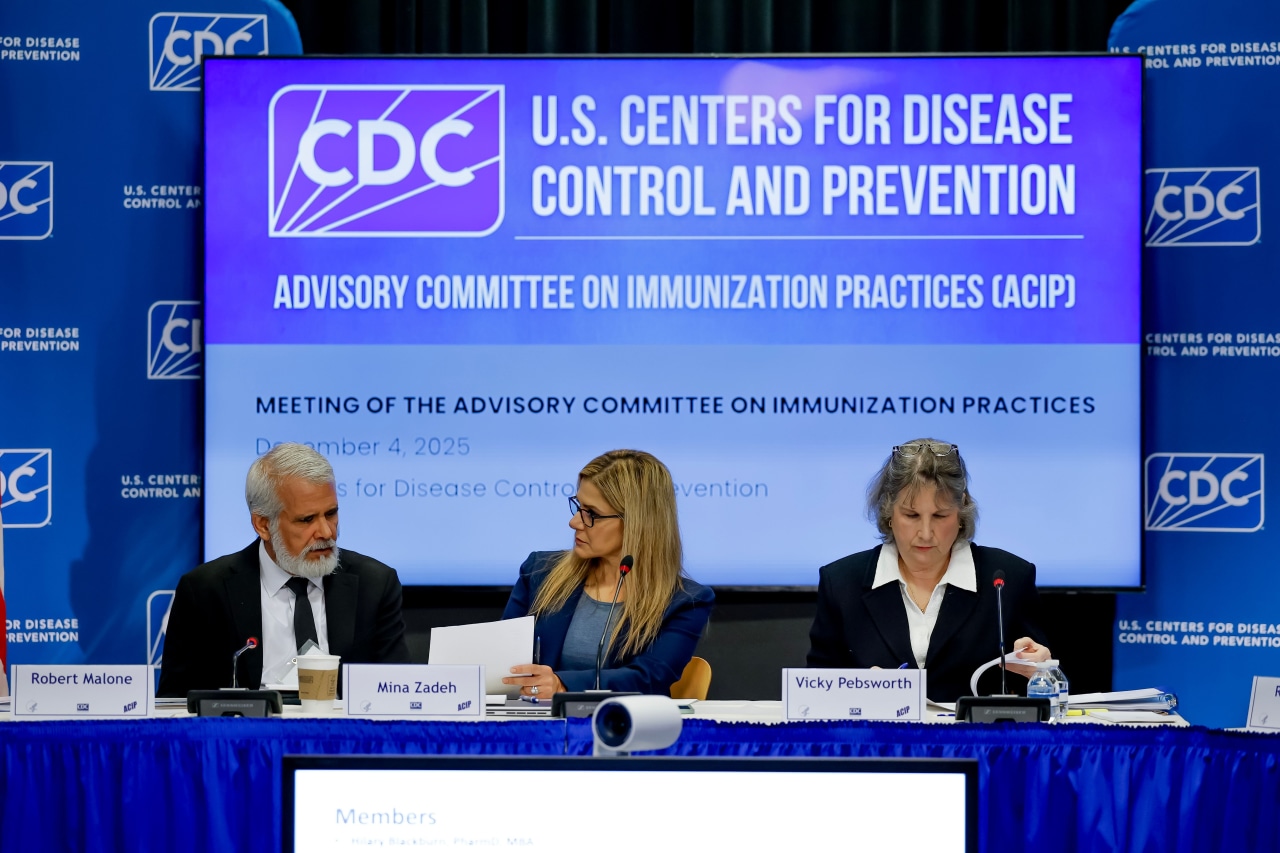
The panel voted 8-3 on Friday after deliberating with presentations from those skeptical of vaccines. This reversal dismisses guidance maintained since 1991, which has been credited with significantly reducing hepatitis B infection rates—an infection that can cause severe liver issues, cancer, and even death.
The Advisory Committee on Immunization Practices (ACIP) now suggests that if a newborn’s mother tests negative for hepatitis B, parents should consult with a healthcare provider about the necessity of administering an early vaccine dose. Additionally, those infants who miss the initial dose at birth should wait until they are at least two months old before receiving their first shot.
This new recommendation, which stems from Health Secretary Robert F. Kennedy Jr.’s earlier reorganization of the panel, still requires approval from the acting CDC director before it can be implemented.
Supporters of the change express concerns that not enough is known about the vaccine’s potential risks, and they believe the likelihood of most babies contracting the virus is relatively low. One committee member, Dr. Evelyn Griffin, raised the possibility that the vaccine might trigger autoimmune disorders, albeit without backing from high-quality research.
“Many parents don’t realize their babies are receiving multiple medical interventions shortly after birth,” stated Griffin, an obstetrician who voted for the change. “This infringes on parental rights.”
However, detractors of the vote criticize the committee for ignoring extensive randomized studies and over three decades of evidence supporting the safety of the birth dose. They argue that monitoring systems for vaccines in the U.S. have found no unusual risks associated with it.
Dr. Joseph Hibbeln, a psychiatrist who opposed the amendment, declared that the committee was remiss in not reviewing the science that justifies a delay in vaccination until two months. He described the committee’s actions as “unconscionable” and demanded more rational discourse.
Experts in public health warn that postponing the vaccine or limiting it solely to infants of infected mothers could pose risks. They remind us that hepatitis B screening is typically performed during the first trimester, which means women could still contract the virus later without being tested. Furthermore, the virus can spread through shared items such as washcloths and toothbrushes, complicating prevention efforts.
Chari Cohen, president of the Hepatitis B Foundation, argues for the importance of the birth dose, highlighting that hepatitis B is the world’s leading cause of liver cancer. “This is not a virus to risk for your newborn,” she emphasized.
During the Thursday session, several speakers introduced ideas related to the anti-vaccine movement. These included ACIP member Vicky Pebsworth from the National Vaccine Information Center, among others who have ties to vaccine skeptics.
The newly appointed acting director of the FDA’s drug division, Dr. Tracy Beth Hoeg, indicated to the panel that hepatitis B vaccines may not be necessary for children at all, referencing the practices of countries like Denmark that don’t promote the vaccine for all newborns. CDC scientist Adam Langer noted that nations like Denmark have strong national health systems that facilitate effective tracking and testing of infected mothers.
Mark Blaxill argued for the beliefs regarding vaccine injury, referencing compensation claims paid out by the National Vaccine Injury Compensation Program. However, federal sources remind us that such settlements should not be used to draw conclusions on vaccine safety.
Dr. Jason Goldman, who represents the American College of Physicians, accused the leadership of the committee of pushing an anti-vaccine agenda. He cautioned against using selective data from individuals lacking scientific rigor to form opinions.
After delaying the vote from Thursday to allow for deeper discussion, the committee voted on the hepatitis B recommendation. Questions arose around the clarity of the vote language, which the CDC had altered shortly before the meeting, leading to confusion among panel members.
ACIP guidelines inform what vaccines are covered free of charge by insurers and government health programs. Some private insurers could potentially stop covering the birth dose for certain infants, although federal insurance programs are expected to maintain coverage for the dose.
The committee also narrowly voted in favor of suggesting that insurance plans cover antibody testing for kids after hep B vaccination to judge if they need additional doses. Generally, hepatitis B vaccines are administered in a series of three doses.
Feel free to get in touch with Liz Essley Whyte at liz.whyte@wsj.com or Sabrina Siddiqui at sabrina.siddiqui@wsj.com.