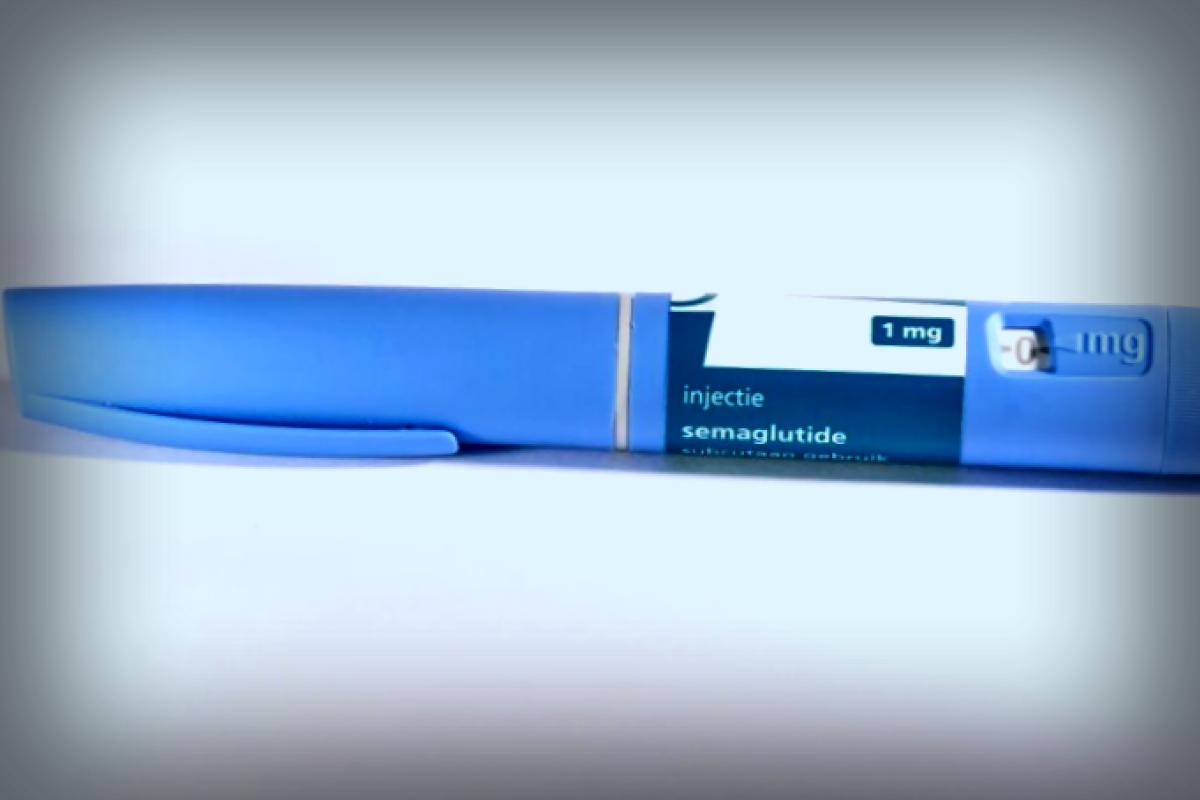
According to a recent panel of international experts featured in The BMJ, adults with type 2 diabetes who are at increased risk of heart and kidney complications should be prescribed SGLT-2 inhibitors and GLP-1 receptor agonists. This recommendation aims to help a broad range of patients manage their health better.
However, for those who fall into the lower risk category, the experts advise that these medications should not be a default option. Instead, it’s better for healthcare providers to discuss various treatment choices with their patients to find what suits them best.
For individuals with diabetes along with chronic kidney disease who are at higher risk, the drug finerenone is recommended due to its benefits potentially outweighing any associated risks. Yet, the use of finerenone isn’t advised for those identified as being at moderate risk.
When it comes to patients battling diabetes and obesity, weight loss becomes crucial. The experts suggest the use of tirzepatide, highlighting its effectiveness in shedding pounds regardless of the patient’s risk level for cardiovascular or kidney issues.
However, the decision between GLP-1 receptor agonists and tirzepatide is nuanced. Doctors should assess the cardiovascular and kidney benefits linked to GLP-1 receptors versus the considerable weight loss results tied to tirzepatide. Understandably, this choice hinges on the patient’s individual health profile and personal preferences.
It’s important to note that for those at high risk of cardiovascular and kidney complications, tirzepatide isn’t intended to replace effective risk-reduction medications. For instance, if a patient transitions from a GLP-1 receptor agonist, additional medications that likewise minimize these risks should still be incorporated.
These evolving practice guidelines are part of The BMJ’s “Rapid Recommendations” initiative, which aims to provide timely and reliable advice rooted in the latest research, assisting doctors in making informed decisions alongside their patients.
The guidelines utilize the GRADE methodology to ensure the credibility of evidence and build organized recommendations. There’s even an interactive decision aid (MATCH-IT) designed to enhance shared decision-making.
These recommendations are drawn from a comprehensive systematic review and network meta-analysis encompassing nearly half a million adults with type 2 diabetes, spread across 869 controlled trials. These studies examined 63 medications and highlighted 26 outcomes that are of particular significance to patients.
Moreover, the panel acknowledges that the availability or high costs of some medications might pose barriers, influencing how these recommendations are implemented in various healthcare settings.
“Every country is trying to keep pace with the influx of new treatments and studies. This extensive systematic review is evidence of the necessity for global cooperation on evidence that supports policy and practice, similar to what we achieved during the COVID-19 pandemic,” commented Professor Per Olav Vandvik, a senior author of the study.
The authors also advocate for the re-use, modification, and translation of these dynamic guidelines via international initiatives like the Alliance for Living Evidence (ALIVE) and the Evidence Synthesis Infrastructure Collaborative (ESIC).
Lastly, the expert panel commits to regularly revisiting and updating these recommendations as new evidence comes to light, supporting informed healthcare practices across the world.
For More Information: Rapid Recommendation: Cardiovascular, Kidney Related, and Weight Loss Effects of Therapeutics for Type 2 Diabetes: A Living Clinical Practice Guideline, BMJ (2025). DOI: 10.1136/bmj-2024-082071
Provided by British Medical Journal